In the hospital on intensive care, you or your relative may encounter different tubes and lines that the medical team use to aid with treatment and care. It can be overwhelming seeing many tubes and devices attached to you or your relative so here’s a simple guide to help understand what they are, why they’re used, and the potential risks.
Central Lines:

What is a central line?
A central line is a thin tube about 20cm long inserted into a large vein, usually in the chest or neck, and ending near the heart. This allows for the delivery of medicines, fluids, blood and nutrition. It also sometimes allows us to take blood samples if other routes are not appropriate. It’s called a central line because it it placed in a large or “central” vein.
What are the benefits?
• Provides easy access for giving important medications and fluids long term.
• Reduces the need for multiple needle pricks for cannulas and blood tests.
• Allows for delivery of medications that can irritate smaller veins and so is given in larger veins.
What are some potential risks?
• Central lines can sometimes feel uncomfortable.
• Infection at the insertion site, with a small risk of this spreading into the bloodstream.
• Blood clots forming in the vein.
• A collapsed lung (this is only a risk during insertion of the line).
How long might this stay in for?
It will remain as long as needed based on your individual treatment plan, anything from a few days to several months. After about 1 week the central line will be reviewed and may be changed for a new one, if it is still needed. Sometimes it’s changed to a different type of line called a ‘PICC’ line (peripherally inserted central cannula).
What can I do to help?
Please let the staff on the ward know if you notice that the dressing has become loose or if the site looks dirty. Additionally, if there is any redness, pain or swelling, please let us know. These changes might be a sign of infection and the line may need replacing or removing.
Arterial Lines

What is an arterial line?
A thin tube inserted into a blood vessel (artery) in the wrist or groin, used to monitor blood pressure continuously and to take blood samples.
What are the benefits?
• Provides accurate and continuous blood pressure monitoring.
• Allows for frequent blood sampling without repeated needle sticks.
What are some potential risks?
• Can be painful to insert, but a local anaesthetic is used to reduce this.
• Infection at the insertion site.
• Bleeding or damage to the artery (less than 1 in every 1000 patients).
How long might this stay in for?
As long as needed for monitoring your blood pressure, it may be replaced 5-10 days after insertion.
What can I do to help?
Please let the staff on the ward know if you notice any redness, pain or swelling, as this might be a sign of infection and the line may need replacing or removing.
Peripherally Inserted Central Catheter (PICC) Lines
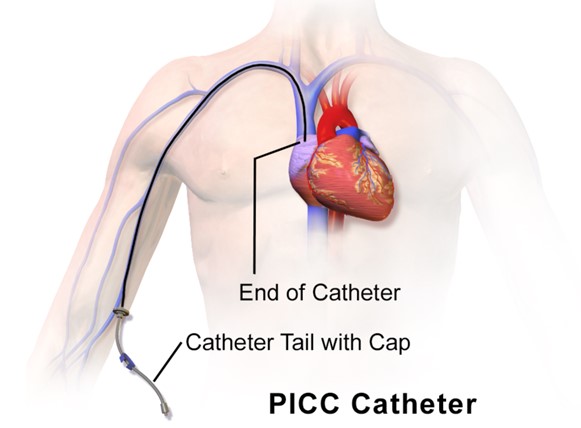
What is a PICC line?
A long flexible tube inserted into a large vein in the arm, with the tip reaching to just outside the heart. It is used when long term access for medications, nutrition or fluids is needed.
What are the benefits?
• Long term reliable access to the bloodstream to give important medications and nutrition.
• Lower risk of infections compared to central lines.
What are some potential risks?
• May still become infected either at the site or in the bloodstream.
• If the PICC line moves or gets damaged it may need to be replaced.
• Blood clots forming in the vein, causing a painful swollen arm.
How long might this stay in for?
PICC lines can stay in place for several weeks or months but they are removed as soon as they are no longer needed.
What can I do to help?
Please let the staff on the ward know if you notice any redness, pain or swelling, as this might be a sign of infection and the line may need replacing or removing. Also tell the staff if you feel your arm is becoming swollen of is uncomfortable.
Endotracheal Tube (E.T. Tube)
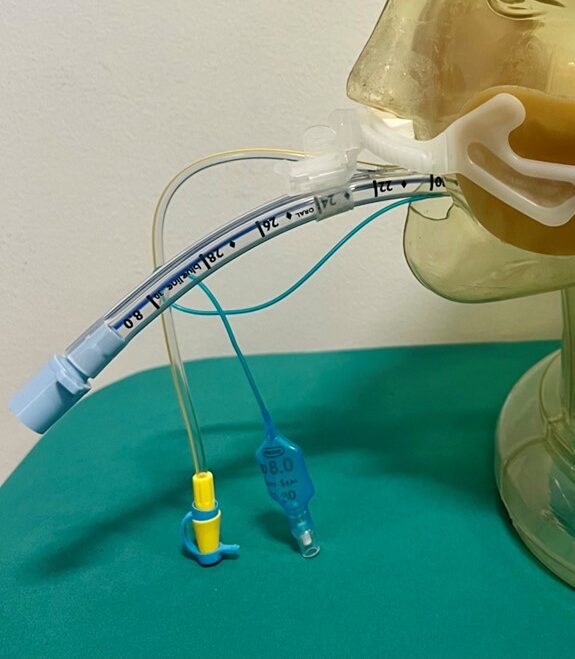
What is an Endotracheal Tube (E.T. Tube) ?
Also known as a breathing tube, it is a tube placed into the windpipe through the mouth, attached to a ventilation machine, helping air get into and out of the lungs. The process of placing the ET tube is known as ‘intubation’. The ET tube is used to protect the airway or if you are struggling to breathe on your own.
What are the benefits?
• To ensure enough oxygen gets to your lungs and carbon dioxide is removed.
• Allows patients to be connected to a breathing machine, to allow doctors to control your breathing.
• Protects lungs from any stomach contents or vomit.
• Prevents the tongue from blocking your airway.
What are some potential risks?
• Most people are not awake whilst this tube is in place, as they can be uncomfortable.
• Once the tube is removed you may experience a hoarse voice, coughing or discomfort, this usually only lasts a few hours.
• May cause damage to the teeth, mouth, or throat during insertion.
• Risk of an infection or a collapsed lung.
• The tube can get blocked or fall out, for this reason there are always doctors and nurses around and multiple alarms to detect these complications.
How long might this stay in for?
It will be removed once you are alert and stable enough to safely breathe on your own. It may be changed if there is anything blocking the tube or if a different size is needed. You may expect this to stay in for 1-2 weeks, if needed for longer then we will consider changing this to a tracheostomy tube.
What can I do to help?
Please let a staff member know if you think the tube has moved or you can hear gurgling or bubbling sounds. If the patient appears to be struggling to catch their breath, please let us know. It may need to be replaced, adjusted or suctioned to removed secretions.
Nasogastric Tubes


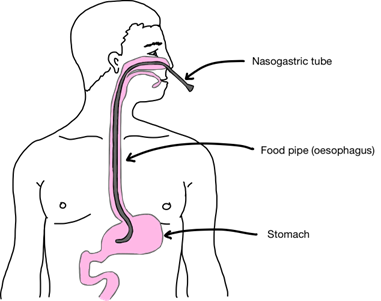
What is a nasogastric tube (N.G. Tube) ?
A thin flexible tube inserted through your nose and down your throat into your stomach. It’s used to deliver food and medication, or it may be used to remove fluids from your stomach.
How is it held in place?
The nasogastric tube may be held in place by tape. If this is done the tube is more likely to become displaced and have to re-sited. It can also be held in place by a “nasal bridle”, this is a strong piece of tape that goes through the back of the nose. It is much more reliable and the tube is less likely to be displaced but it may be more uncomfortable. If the tube is displaced before it is time to come out it will most likely have to be replaced.
What are the benefits?
• Gives nutrition and hydration if you are unable to eat or drink normally or safely.
• Can remove built up stomach fluids if needed.
• Allows us to give medicines if you are unable to swallow.
What are some potential risks?
• Discomfort and irritation in the nose and throat.
• Nosebleeds or damage to the nasal passages (only during insertion).
• If the nasogastric tube becomes displaced into the patients lungs this could be very dangerous, for this reason we regularly check these tubes.
How long might this stay in for?
It will be removed when you are safe to eat and drink, which is usually decided by the speech and language therapists (SALT). This may be after several days or as long as it is needed.
What can I do to help?
Let a member of staff know if you notice any discomfort or you believe the tube has moved.
If you believe the tube has moved, your nose is getting sore or it is tugging on your nose please let us know. If you are visiting explain to the patient why they need the tube and should keep it in (this nurses will have done this but sometimes patients pay more attention to relatives!)
Urinary Catheters
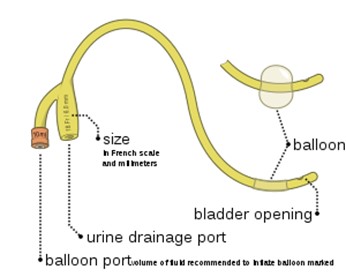
What is a Urinary Catheter ?
A thin flexible tube inserted into the bladder through the hole that normally drains urine (urethra). This tube allows urine to drain from the bladder into a collection bag, when you’re unable to do so on your own.
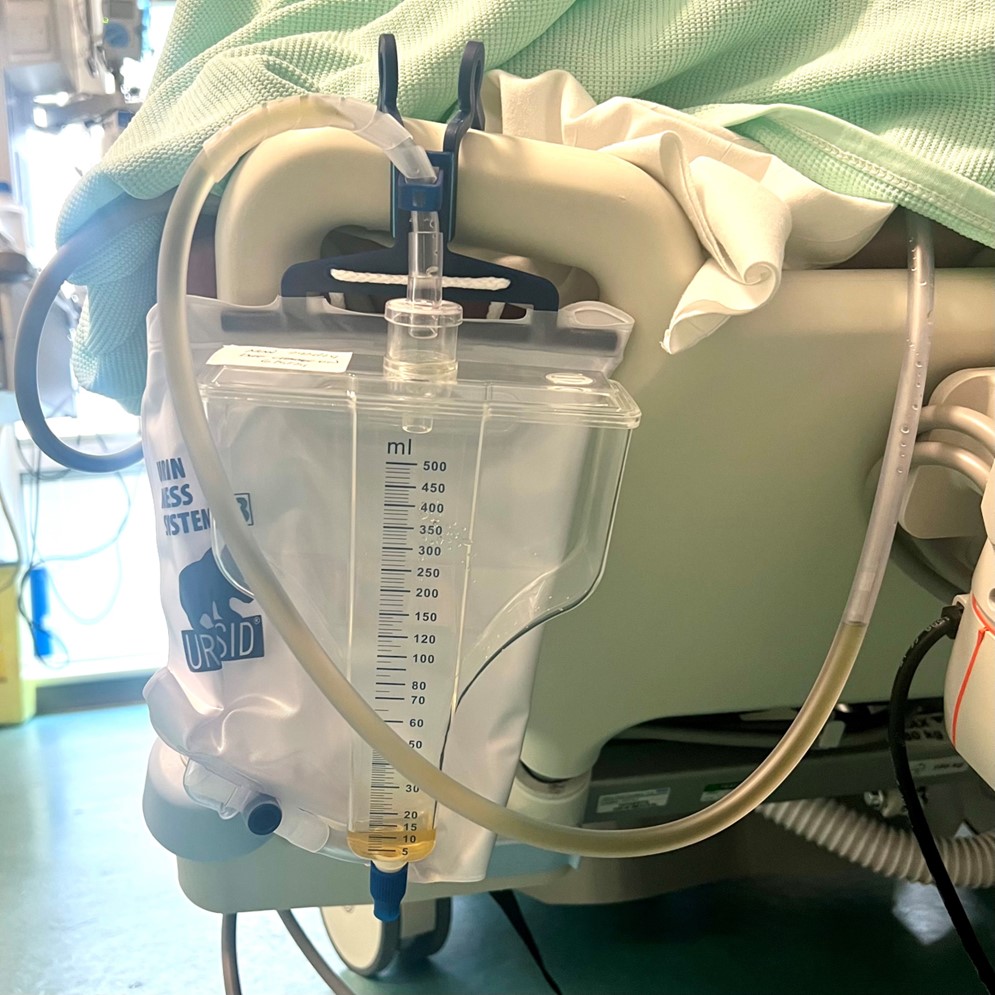
What are the benefits?
• Prevents urinary retention (inability to empty the bladder).
• To monitor how much urine is produced accurately.
What are some potential risks?
• Infections of the urethra, bladder or kidneys (UTI’s).
• Injury to the bladder during insertion.
• May cause discomfort and irritation.
How long might this stay in for?
Urinary catheters can stay in place for several weeks before needing to be changed. They will be removed once you are able to use the toilet or bed pan independently.
What can I do to help?
Let us know when you feel ready to be without the catheter or are getting any pain, discomfort or it is not draining correctly.
If you are the relative, sometimes patients don’t realise they have a urinary catheter in, they feel as if they need to pass urine so please reassure them that they have a tube helping them to do this.
Chest Drains

What is a chest drain?
The lungs have a thin layer of fluid over them that allows them to move smoothly in your chest as you breath. This fluid is held in a small space called the pleural space. Air or fluid may get into this pleural space and cause the underlying lung to collapse. In this situation a “chest drain” is placed in the pleural space to drain the fluid or air and allow the lungs to re-open. In our unit air normally gets into the pleural space following an accident where the lungs are damaged and they leak air. This is also the most common reason for blood in the space. Pus normally collects as a complication of pneumonia, other fluid collects for many different reasons. In our unit chest drains are also commonly left in after the operation of oesophagectomy. This is because fluid would otherwise collect around the operation site, if there is a complication of this surgery the fluid draining out often changes colour to warn us to look for problems that we can then sort out.
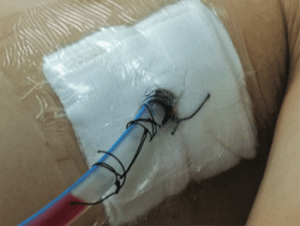

The fluid or air coming out of the drain goes into a bottle, this has water at the bottom of it and the drain opens into this water. This allows the air or fluid to come out but stops air going the wrong way up the tube into the pleura. The bottle must be kept below the chest and must be kept upright or air or fluid could go the wrong way into the pleura.


What are the benefits?
To allow fluid or air to drain away from the lining of the lung to allow it to expand properly. Leaving fluid or blood around the lung could allow scaring or abscess to develop.
What are the risks?
There are risks in placing the drain in terms of bleeding, misplacement into the lung and pain during placement. The chances are that the drain will already have been placed by the time you read this. After placement the main risks are that the tube could fall out or become disconnected, so allowing air to get into the pleural space. The drains are uncomfortable and make it difficult to cough. If the tubing kinks it won’t work.
How long will it stay in for?
Most drains stay in for a few days or a week. It will depend on the underlying problem being sorted. Sometimes air continues to leak from a pneumothorax and the drain has to be attached to a suction device on the wall behind the bed.
When the drain is removed the stiches holding it are cut and it is gently pulled out and a dressing is placed over the hole. The hole will quickly heal leaving a small coin sized scar.
What can I do to help?
Tell the nurse if the drain is painful. Make sure the drain bottle stays below your chest. If you think the drain may be kinked or have disconnected at any of the joins then tell the nurse straight away. If the drain bottle falls over put it straight and tell the nurse. Deep breaths and coughing will help re-expand the lungs. The nurses and physiotherapists may encourage you to walk around your bed area or the unit with the drains in. This is good as it speeds your recovery, but make sure you follow their instructions to keep the drains safe.